Study: Stem cells used to reverse woman’s type 1 diabetes
In a groundbreaking medical breakthrough, a 25-year-old woman with type 1 diabetes has successfully reversed her condition after receiving a transplant of reprogrammed stem cells. This marks a world first, as the cells used were extracted from her own body, enabling her to produce insulin naturally. Her case provides a promising glimpse into the future of diabetes treatment and offers hope to millions affected by the disease worldwide.
"I can eat sugar now," the woman shared in a conversation with Nature, describing how her life has changed since the transplant. It's been over a year, and she now enjoys all types of food, especially hotpots, without needing to manage blood sugar levels with insulin.
How does it work?
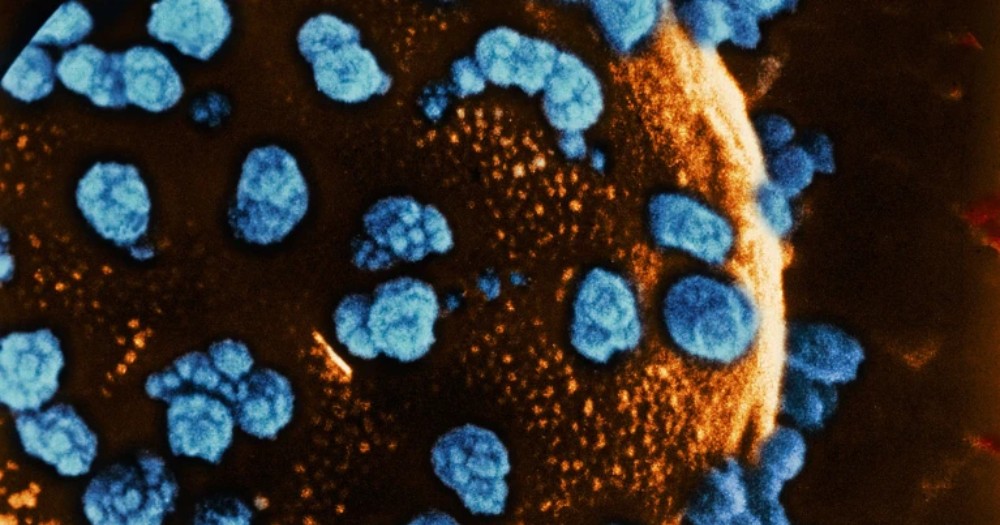
This revolutionary treatment stems from advances in stem cell technology, specifically using reprogrammed cells from the patient's own body. The procedure, led by Deng Hongkui, a cell biologist from Peking University, involved reverting cells to a pluripotent state — allowing them to develop into any cell type, including insulin-producing islet cells. This method was built on work pioneered by Shinya Yamanaka two decades ago but was further refined by using small molecules for more precise control.
The team generated 3D clusters of islets from these pluripotent cells and transplanted them into the woman's abdominal muscles. This location, unlike the liver (a common site for islet transplants), allowed the researchers to monitor the cells' activity using MRI and potentially remove them if necessary. Remarkably, within just two and a half months of the procedure, the woman was producing sufficient insulin, eliminating her need for external insulin doses.
Why does it matter?
This achievement matters profoundly because it tackles a major issue with diabetes treatment: the shortage of donor islet cells and the need for immunosuppressants to prevent rejection. By using stem cells reprogrammed from the patient's own body, this approach ensures a limitless supply of islet cells while also holding the potential to eliminate the need for lifelong immune suppression — a critical hurdle in conventional transplant medicine.
As James Shapiro, a transplant surgeon from the University of Alberta, noted, "They've completely reversed diabetes in the patient, who was requiring substantial amounts of insulin beforehand."
For people with type 1 diabetes, whose immune systems attack their pancreatic islet cells, this offers a novel, potentially safer solution that could change the landscape of diabetes care. If these results can be replicated in more patients, the benefits will be far-reaching — offering an alternative for the nearly half a billion people living with diabetes globally.
The context
The field of diabetes research has been exploring stem cell therapies for years, with promising strides made in both type 1 and type 2 diabetes cases. Previous efforts have included transplanting insulin-producing islet cells into the liver, as demonstrated by a study in Shanghai, where a 59-year-old man with type 2 diabetes stopped taking insulin after receiving a similar treatment. However, the scarcity of donor islets and the need for immunosuppressants remained significant challenges.
This new approach using pluripotent stem cells presents a potential game-changer. While scaling up and commercializing the process using a patient's own cells remains complex, researchers are now exploring alternative methods. Trials like those by Vertex Pharmaceuticals are investigating the use of donor-derived stem cells with the hope of making this treatment widely accessible.
Future steps include more trials and developing ways to protect transplanted cells from autoimmune attacks, which are still a concern in type 1 diabetes. Though it's early, the implications of this breakthrough are vast and may lead to safer, more effective treatments for diabetes in the near future.
💡Did you know?
You can take your DHArab experience to the next level with our Premium Membership.👉 Click here to learn more
🛠️Featured tool
 Easy-Peasy
Easy-Peasy
An all-in-one AI tool offering the ability to build no-code AI Bots, create articles & social media posts, convert text into natural speech in 40+ languages, create and edit images, generate videos, and more.
👉 Click here to learn more


